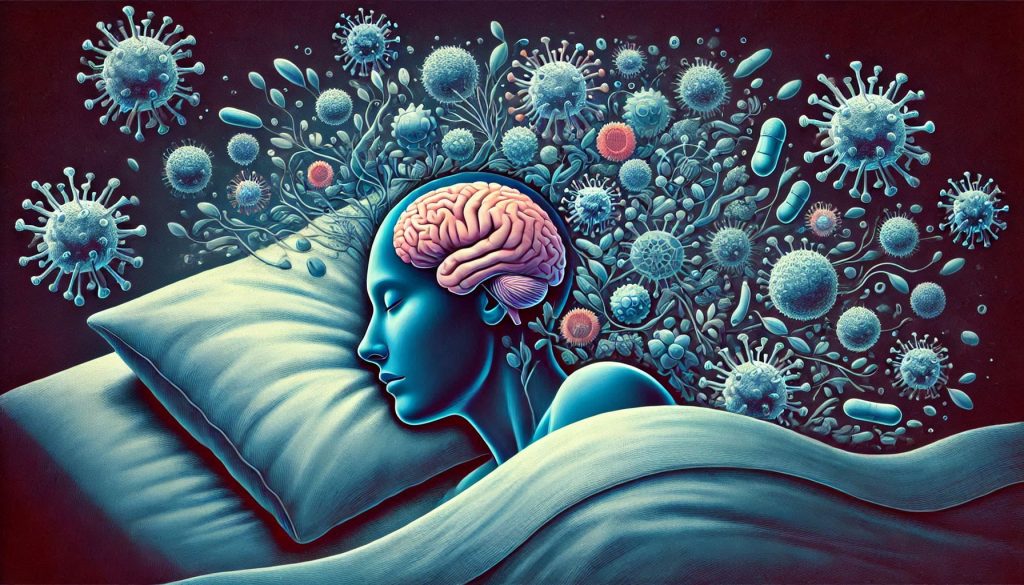
Sleep, an essential pillar of health, plays a fundamental role in regulating the immune system. While its restorative properties are often associated with cognitive and emotional well-being, emerging research underscores its pivotal impact on physical health, particularly immunity. From influencing the body’s ability to fend off infections to modulating chronic inflammation, sleep is intertwined with the complex mechanisms that sustain immune resilience. This article delves into the multidimensional relationship between sleep and the immune system, uncovering how quality rest fortifies our defenses and what happens when sleep is compromised.
The Basics: How Sleep Influences the Immune System
Sleep is a biologically conserved process that influences various physiological functions, including the immune response. During sleep, the body enters a state of repair and rejuvenation, with critical processes taking place to bolster immune defenses:
Cytokine Production:
- Cytokines are proteins that regulate immune responses. During sleep, particularly deep sleep (slow-wave sleep), the production of certain cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), is unregulated. These molecules are essential for combating infections and inflammation.
Lymphocyte Function:
- Sleep enhances the activity of lymphocytes, particularly T-cells, which are critical for identifying and neutralizing pathogens. Recent studies highlight that sleep facilitates integrin activation in T-cells, enabling them to attach to infected cells more effectively.
Hormonal Regulation:
- Hormones such as cortisol and melatonin, which follow a circadian rhythm, significantly influence immune function. During sleep, cortisol levels decrease, reducing immune suppression, while melatonin—an antioxidant—supports immune cell activity. This harmonious balance underpins the body’s ability to manage threats effectively.
Acute Sleep Deprivation: Immediate Effects on Immunity
Even a single night of inadequate sleep can disrupt immune system function. Acute sleep deprivation impacts the body in several ways:
Reduction in Natural Killer (NK) Cells:
- NK cells play a crucial role in the early defense against viruses and tumor cells. Sleep deprivation has been shown to reduce their activity by up to 70%, leaving the body vulnerable to infections. This highlights the critical role of even short-term sleep in maintaining immunity.
Impaired Vaccine Response:
- Studies reveal that individuals who experience sleep deprivation before or after receiving a vaccine produce fewer antibodies, undermining the vaccine’s efficacy. This has significant implications for public health, especially during global immunization campaigns.
Increased Inflammatory Markers:
- A lack of sleep leads to elevated levels of C-reactive protein (CRP) and other inflammatory markers, which can exacerbate the risk of developing chronic inflammatory diseases. The inflammatory environment also strains other physiological systems, such as cardiovascular health.
Chronic Sleep Deprivation: Long-Term Immune Consequences
Chronic sleep deprivation—defined as consistently obtaining less than the recommended 7-9 hours of sleep—exerts profound effects on immune function, with implications for overall health:
Heightened Risk of Infections:
- Chronic sleep deprivation impairs the body’s ability to mount an effective immune response, increasing susceptibility to respiratory infections such as the common cold and influenza. Repeated infections can have a compounding effect, further weakening immunity over time.
Autoimmune Deregulation:
- Persistent sleep disturbances can contribute to autoimmune disorders by promoting systemic inflammation and impairing immune tolerance. Conditions such as rheumatoid arthritis and lupus have been linked to poor sleep quality.
Cancer Progression:
- Disrupted sleep patterns, such as those seen in shift workers, are associated with a higher risk of cancer. This link may stem from impaired NK cell activity and circadian rhythm disruption, emphasizing the need for targeted interventions in high-risk groups.
Accelerated Aging of the Immune System:
- Sleep deprivation accelerates immunosenescence, the age-related decline in immune function, increasing vulnerability to infections and reducing the efficacy of vaccinations in older adults. This highlights the importance of prioritizing sleep across all life stages.
The Role of Circadian Rhythms in Immune Health
The immune system operates in harmony with the body’s circadian rhythms, the natural 24-hour cycles that govern physiological processes. Sleep disturbances can disrupt this synchronization, leading to:
Misaligned Immune Responses:
- Circadian misalignment, such as that caused by shift work or jet lag, disrupts the timing of cytokine production, impairing the body’s ability to respond to pathogens effectively. This misalignment can also impact energy levels, reducing overall resilience.
Impaired Chronopharmacology:
- Medications targeting the immune system, including immunosuppressants and vaccines, are influenced by circadian timing. Disrupted sleep can reduce their efficacy. Optimizing treatment schedules to align with circadian patterns could revolutionize immune therapy.
Special Populations: Sleep and Immune Health in Vulnerable Groups
Children and Adolescents:
- Sleep is critical during developmental years, as the immune system is still maturing. Poor sleep in children is linked to increased rates of infections, allergies, and autoimmune conditions. Addressing sleep in this demographic is crucial for lifelong health benefits.
Older Adults:
- Aging naturally diminishes sleep quality and immune function. Strategies to improve sleep in older adults, such as cognitive-behavioral therapy for insomnia (CBT-I), can enhance immune resilience. This can have significant implications for reducing age-related health disparities.
Individuals with Chronic Illnesses:
- Chronic conditions such as diabetes, cardiovascular disease, and obesity often coexist with poor sleep and compromised immunity. Addressing sleep issues in these populations is vital for improving health outcomes and managing comorbidities effectively.
Optimizing Sleep for Immune Health
Enhancing sleep quality is one of the most accessible ways to support immune resilience. Practical strategies include:
Establishing a Consistent Sleep Schedule:
- Going to bed and waking up at the same time daily reinforces circadian rhythms. This consistency is vital for optimizing immune cycles.
Creating a Sleep-Conducive Environment:
- A dark, quiet, and cool bedroom promotes restorative sleep. Reducing exposure to screens and blue light before bedtime is also crucial. Investing in blackout curtains or white noise machines can also enhance the sleep environment.
Prioritizing Sleep Hygiene:
- Practices such as avoiding caffeine and heavy meals in the evening, as well as incorporating relaxation techniques, can improve sleep quality. Activities such as reading or meditating before bed help the mind and body prepare for rest.
Leveraging Nutrition:
- Certain foods, such as those rich in magnesium, tryptophan, and melatonin (e.g., nuts, bananas, and tart cherries), can promote better sleep. Hydration and timing of meals also play roles in sleep optimization.
Managing Stress:
- Chronic stress disrupts sleep and suppresses immune function. Mindfulness, yoga, and therapy can help mitigate stress-induced sleep disturbances, ensuring a robust immune defense.
Future Directions: Research and Innovations
The field of sleep and immunity continues to evolve, with exciting areas of research, including:
Chronotherapy:
- Timing interventions, such as medications and vaccines, to align with circadian rhythms for maximum efficacy. This could optimize immune responses and reduce side effects.
Wearable Technology:
- Devices that monitor sleep patterns and provide personalized recommendations for improving sleep quality and immune health. These innovations make sleep optimization accessible and actionable.
Micro biome-Sleep Interactions:
- Investigating how gut bacteria influence sleep and immunity, with potential for probiotic-based interventions. The micro biome is emerging as a critical player in the sleep-immune axis.
Targeted Therapies for Shift Workers:
- Developing strategies to mitigate the immune and sleep challenges faced by individuals with irregular work schedules. Interventions could include light therapy, dietary modifications, or specialized supplements.
Conclusion
Sleep is not merely a state of rest; it is an active process that orchestrates the body’s defense mechanisms. From enhancing cytokine production to fortifying adaptive immune responses, quality sleep is integral to immune resilience. Conversely, sleep deprivation compromises these processes, leaving the body vulnerable to infections, chronic diseases, and immune deregulation. Prioritizing sleep as a cornerstone of health is essential, both at an individual level and in public health initiatives. As research advances, understanding and harnessing the sleep-immunity connection will unlock new avenues for enhancing overall well-being and resilience in an increasingly demanding world.
SOURCES
Irwin, M. R., & Pop, M. R. (2017). “Sleep and Immunity: The Role of Cytokines in Health and Disease.” Nature Reviews Immunology, 17(11), 733-744.
Besedovsky, L., Lange, T., & Born, J. (2012). “Sleep and Immune Function.” Plungers Archive – European Journal of Physiology, 463(1), 121-137.
Dimitrov, S., Lange, T., & Born, J. (2019). “Sleep’s Role in the Regulation of Systemic Immunity.” Advances in Experimental Medicine and Biology, 1193, 65-83.
Irwin, M. R., Wang, M., Camp mayor, C. O., Collide-Hidalgo, A., & Cole, S. (2006). “Sleep Deprivation and Activation of Morning Levels of Cellular and Genomic Markers of Inflammation.” Archives of Internal Medicine, 166(16), 1756-1762.
Spiegel, K., Sheridan, J. F., & Van Cautery, E. (2002). “Effect of Sleep Deprivation on Response to Immunization.” Journal of the American Medical Association, 288(12), 1471-1472.
Patel, S. R., Zhu, X., Storfer-Isser, A., Mehta, R., Jenny, N. S., Tracy, R., & Redline, S. (2009). “Sleep Duration and Biomarkers of Inflammation.” Sleep, 32(2), 200-204.
Prather, A. A., & Leung, C. W. (2016). “Association of Insufficient Sleep with Respiratory Infection among Adults in the United States.” JAMA Internal Medicine, 176(6), 850-852.
Shire, R., & Koskimäki, J. (2015). “Chronic Sleep Problems and Risk of Autoimmune Disease: A Prospective Cohort Study.” Psychosomatic Medicine, 77(8), 867-874.
Sigurdardóttir, L. G., et al. (2012). “Sleep Disruption and Cancer Risk: Results from the Reykjavik Study.” Cancer Epidemiology, Biomarkers & Prevention, 21(6), 887-894.
Cohen, S., Janicki-Deverts, D., Turner, R. B., & Doyle, W. J. (2015). “Chronic Stress, Sleep Deprivation, and Susceptibility to the Common Cold.” Health Psychology, 34(11), 1185-1191.
Schliemann, C., Kunisaki, Y., & Frenette, P. S. (2013). “Circadian Control of the Immune System.” Nature Reviews Immunology, 13(3), 190-198.
Smolensky, M. H., Hermida, R. C., & Portaluppi, F. (2017). “Chronotherapy and the Timing of Medication in Cardiovascular and Immune Diseases.” Current Opinion in Pharmacology, 33, 35-42.
Miller, M. A., & Wright, H. (2019). “Sleep and Development in Childhood and Adolescence.” Nature and Science of Sleep, 11, 35-50.
Irwin, M. R. (2015). “Sleep and Inflammation: Partners in Sickness and in Health.” Nature Reviews Immunology, 15(4), 260-270.
Knutson, K. L., & Van Cauter, E. (2008). “Associations Between Sleep Loss and Increased Risk of Obesity and Diabetes.” Annals of the New York Academy of Sciences, 1129(1), 287-304.
HISTORY
Current Version
January, 07, 2025
Written By
Asifa