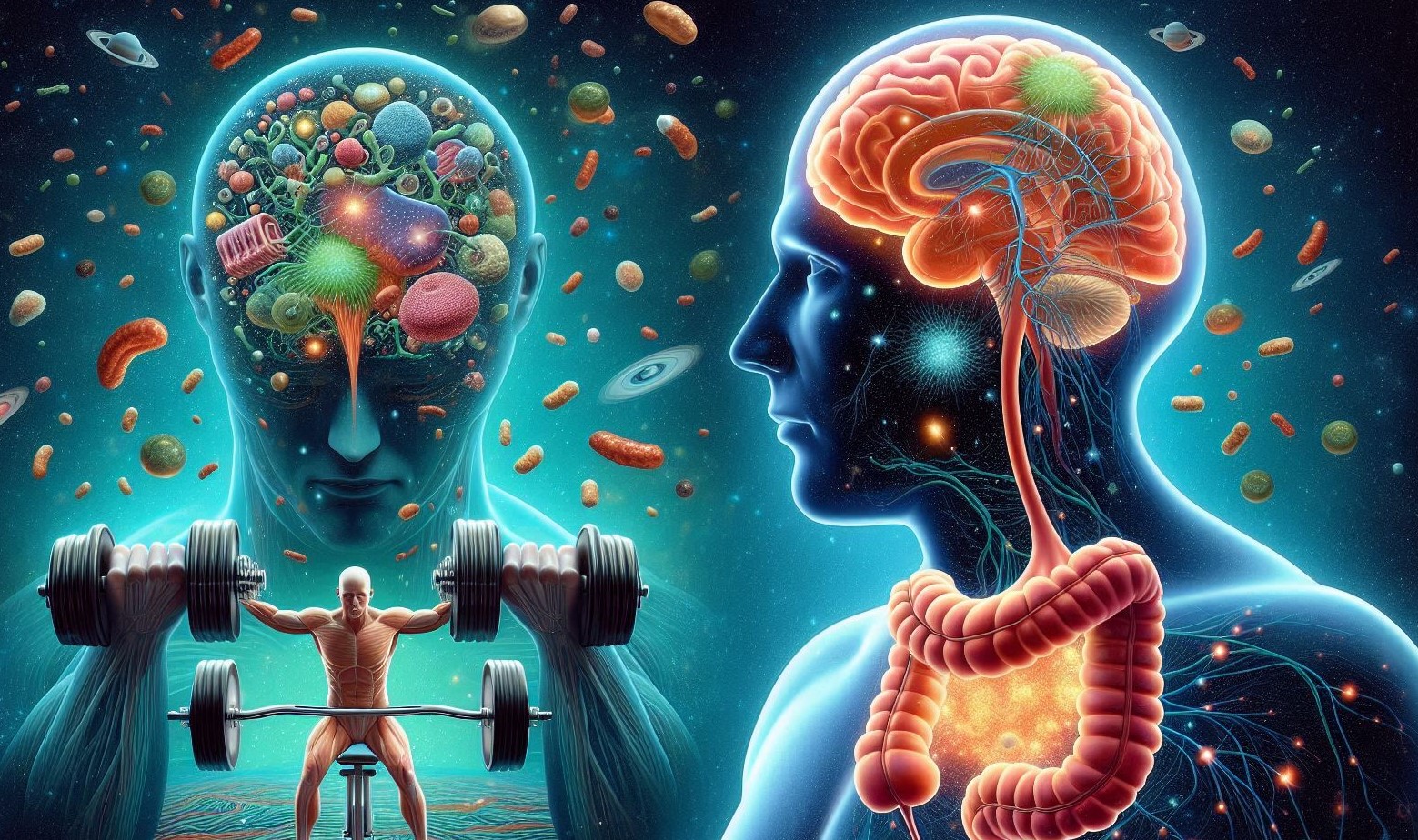
The human body is a complex, interconnected system where a action in one area can create a ripple effect throughout. Nowhere is this more evident than in the dynamic relationship between intense physical exertion and the digestive system—a relationship mediated by a sophisticated network of nerves, hormones, and a vast ecosystem of gut microbes. For athletes and fitness enthusiasts, understanding this mind-gut-microbiome axis is crucial. It holds the key to unlocking peak performance, avoiding debilitating gastrointestinal distress, and harnessing exercise as a powerful tool for long-term health that extends far beyond muscle and cardiovascular fitness.
The Gut: More Than Just a Digestion Factory
To appreciate how exercise impacts the gut, we must first understand its complexity. The gut is often called the “second brain,” a title earned by its own intrinsic nervous system, the Enteric Nervous System (ENS). Comprising over 100 million neurons, the ENS can operate independently but is in constant communication with the central nervous system (CNS) via the vagus nerve. This bi-directional superhighway is the physical core of the mind-gut connection, transmitting signals that influence mood, stress levels, and, crucially, digestive processes.
Lining this system is the gut microbiome, a diverse community of trillions of bacteria, viruses, fungi, and archaea. This is not a passive community; it is an active metabolic organ that influences everything from nutrient extraction and vitamin synthesis (like Vitamin K and B vitamins) to immune system regulation (70-80% of the immune system resides in the gut) and even the production of neurotransmitters like serotonin (about 90% of the body’s serotonin is produced in the gut).
When we engage in intense exercise, we send a shockwave through this delicate ecosystem, triggering a cascade of physiological responses with both immediate and long-term consequences.
The Immediate Impact: Exercise-Induced Gastrointestinal Distress
For many, the most familiar experience of the gut-exercise connection is the unpleasant one: cramping, nausea, reflux, urgency, and even diarrhea during or after a hard workout. This is particularly common in endurance sports like running, cycling, and triathlon, with prevalence rates estimated to affect 30-90% of athletes. The causes are multifactorial and stem from the body’s survival-oriented response to intense physical stress.
- 1. Blood Flow Redistribution (Splanchnic Hypoperfusion): This is the primary driver. During intense exercise, the body faces competing demands. Skeletal muscles and the heart require a massive increase in oxygenated blood to sustain effort. To meet this demand, the body diverts blood away from “non-essential” systems, with the gastrointestinal tract being a major casualty. Blood flow to the gut can be reduced by up to 80%. This ischemia (lack of blood flow) has several consequences:
- Impaired Barrier Function: The gut lining is a single layer of cells held together by tight junctions, acting as a selective barrier. Ischemia and the resulting oxygen deprivation weaken these junctions, potentially leading to a “leaky gut.” This allows endotoxins, like Lipopolysaccharide (LPS) from the cell walls of gram-negative bacteria, to translocate into the bloodstream.
- Nausea and Cramping: Reduced blood flow slows gastric emptying (the process of food leaving the stomach) and intestinal motility. Food and acid sit in the stomach longer, leading to feelings of fullness, bloating, reflux, and nausea. The ischemia itself can also trigger painful cramping.
- Mechanical Jarring and Jostling: High-impact activities like running create a physical “bouncing” effect that jostles the digestive organs. This can aggravate the intestinal lining, accelerate transit time, and contribute to feelings of urgency and diarrhea.
- Neuroendocrine and Stress Response: Intense exercise is a physiological stressor. It activates the sympathetic nervous system (the “fight or flight” system) and the hypothalamic-pituitary-adrenal (HPA) axis, leading to the release of stress hormones like cortisol and catecholamines (e.g., adrenaline). These hormones further inhibit digestive processes, suppressing gastric secretion and motility to prioritize the immediate physical threat (the workout). They can also alter the composition of the gut microbiota in the short term.
- Dietary Triggers: What an athlete consumes before and during exercise interacts dramatically with this stressed system. High-fiber, high-fat, or high-protein foods pre-workout take longer to digest and are more likely to cause distress under conditions of reduced blood flow. Concentrated sugary sports drinks and gels, while providing necessary fuel, create a high osmotic load in the intestine, drawing water into the gut and potentially causing watery diarrhea.
The Long-Term Adaptation: Exercise as a Microbiome Modulator
While the acute effects of intense exercise can be negative, the long-term, chronic adaptations are overwhelmingly positive. This is the paradox of exercise hormesis: a beneficial adaptive response to a mild stressor. Regular physical activity is one of the most powerful lifestyle factors for cultivating a healthy, diverse gut microbiome.
- Increased Microbial Diversity: A hallmark of a healthy gut is a high level of biodiversity—a wide array of different microbial species. Numerous studies have shown that athletes consistently have greater gut microbial diversity compared to sedentary controls (Clark & Mach, 2016; Barton et al., 2018). Diversity is resilience. A more diverse ecosystem is better able to resist perturbations, perform its functions, and protect against pathogen overgrowth.
- Boosting the “Beneficial” Bacteria: Exercise appears to selectively promote the growth of bacteria that produce beneficial compounds, particularly short-chain fatty acids (SCFAs).
- SCFA Production: The most notable SCFAs are acetate, propionate, and butyrate. Butyrate is the primary fuel source for the cells lining the colon, helping to maintain a strong, healthy gut barrier and prevent the “leaky gut” that can occur acutely. All SCFAs have potent anti-inflammatory properties throughout the body. Regular exercise has been linked to increased abundance of SCFA-producing bacteria, such as Faecalibacterium prausnitzii, Roseburia, and Akkermansia muciniphila .
- Akkermansia muciniphila: This bacterium has garnered significant attention as a next-generation probiotic. It thrives on the mucin layer that protects the gut lining, strengthening it and improving metabolic health. Its abundance is positively correlated with exercise levels and inversely correlated with obesity and metabolic disorders.
- Anti-Inflammatory Effects: The SCFAs produced by the exercise-enriched microbiome are crucial signaling molecules. They help regulate the immune system, reducing systemic inflammation. Propionate, for example, can travel to the liver and reduce the expression of pro-inflammatory genes. This creates a positive feedback loop: exercise reduces gut inflammation, which allows for a healthier microbiome, which in turn produces more anti-inflammatory compounds.
- The Tryptophan-Serotonin Connection: Exercise influences the gut-brain axis through neurotransmitter pathways. The gut microbiome plays a key role in the metabolism of the essential amino acid tryptophan. Regular exercise can shift tryptophan metabolism away from the kynurenine pathway (associated with stress and inflammation) and towards the production of serotonin. This not only improves mood but also regulates gut motility and overall gut function.
The Athlete’s Paradox: Managing Acute Distress to Reap Long-Term Gains
The challenge for athletes is to navigate the acute gastrointestinal distress that can hinder performance while pursuing the long-term microbial benefits. This requires a strategic approach:
- 1. Nutrition Periodization:
- Pre-Workout (2-3 hours before): Consume a easily digestible, low-residue meal low in fiber and fat. Focus on simple carbohydrates (e.g., white toast with banana, oatmeal).
- During Workout: Practice your nutrition strategy during training, not on race day. For endurance events, use sports nutrition products (gels, chews) with water and consider isotonic formulas that have a lower osmotic load. Train your gut to handle fuel under stress.
- Post-Workout: The recovery window is critical for gut health. Consume a mix of carbohydrates and protein to replenish glycogen stores and aid muscle repair. Consider incorporating fermented foods (yogurt, kefir) or polyphenol-rich foods (berries, dark chocolate) to support microbial recovery.
- Hydration Strategy: Dehydration exacerbates gut ischemia. Maintain fluid balance with electrolytes before, during, and after exercise. Avoid hypertonic fluids in large quantities during intense effort.
- Stress Management: Since psychological stress can amplify gut issues via the same pathways, incorporating recovery practices like sleep, meditation, and yoga can positively influence gut health and resilience.
- Gradual Progression: Just as you progressively overload muscles, progressively overload your gut. Gradually increase the intensity and duration of your workouts to allow your digestive system to adapt alongside your cardiovascular and muscular systems.
Conclusion
The connection between intense exercise, digestion, and the microbiome is a profound example of the body’s interconnectedness. The acute stress of a hard workout temporarily disrupts gut function, a necessary trade-off for powering muscular performance. However, when applied consistently, this same stressor triggers powerful adaptive responses that enhance microbial diversity, strengthen the gut barrier, and reduce systemic inflammation.
The gut is not a passive spectator to athletic endeavor; it is an active, adaptable organ that, when cared for strategically, becomes a powerful ally in the pursuit of health and performance. By listening to its signals, fueling it intelligently, and respecting the profound link between the mind and the gut, we can harness intense exercise not just to build a stronger body, but to cultivate a healthier, more resilient microbial universe within.
SOURCES
Barton, W., Penney, N. C., Cronin, O., Garcia-Perez, I., Molloy, M. G., Holmes, E., Shanahan, F., Cotter, P. D., & O’Sullivan, O. (2018). The microbiome of professional athletes differs from that of more sedentary subjects in composition and particularly at the functional metabolic level. Gut, 67(4), 625–633.
Clark, A., & Mach, N. (2016). Exercise-induced stress behavior, gut-microbiota-brain axis and diet: a systematic review for athletes. Journal of the International Society of Sports Nutrition, 13, 43.
Estaki, M., Pither, J., Baumeister, P., Little, J. P., Gill, S. K., Ghosh, S., Ahmadi-Vand, Z., Marsden, K. R., & Gibson, D. L. (2016). Cardiorespiratory fitness as a predictor of intestinal microbial diversity and distinct metagenomic functions. Microbiome, 4(1), 42.
Mailing, L. J., Allen, J. M., Buford, T. W., Fields, C. J., & Woods, J. A. (2019). Exercise and the Gut Microbiome: A Review of the Evidence, Potential Mechanisms, and Implications for Human Health. Exercise and Sport Sciences Reviews, 47(2), 75–85.
Scheiman, J., Luber, J. M., Chavkin, T. A., MacDonald, T., Tung, A., Pham, L. D., Wibowo, M. C., Wurth, R. C., Punthambaker, S., Tierney, B. T., Yang, Z., Hattab, M. W., Avila-Pacheco, J., Clish, C. B., Lessard, S., Church, G. M., & Kostic, A. D. (2019). Meta-omics analysis of elite athletes identifies a performance-enhancing microbe that functions via lactate metabolism. Nature Medicine, 25(7), 1104–1109.
HISTORY
Current Version
Sep 6, 2025
Written By:
SUMMIYAH MAHMOOD